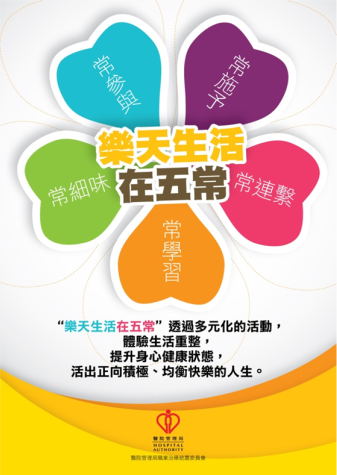
Five elements of a positive life
To help patients to overcome physical, psychological and environmental barriers, active participation in meaningful activities can restore the sense of achievement and joy. With this we hope to ultimately improve the patient’s motivation and quality of life. Five ways include: Connect with other people, Be physically active, Learn new skills, Give to others, Pay attention to the present moment.